This paper was submitted as part of Dr. Torrance's application for ACOFP Fellowship, which recognizes exceptional national, state, and local service through teaching, authorship, research, or professional leadership. Visit the ACOFP Fellows page to learn more about fellowship and the nomination process.
ABSTRACT
Low back pain (LBP) is a frequent cause of sport limitation in young athletes and a common complaint that prompts a visit to a physician’s office. The most common cause of low back pain in the adolescent athlete is isthmic spondylolysis, or a defect of the pars interarticularis. When symptomatic spondylolysis patients fail conservative management, surgery is an option, but is invasive, and can lead to serious complications coupled with a prolonged recovery period, which is not ideal for competitive athletes. A bone marrow aspirate concentrate injection (BMAC) provides a safe, non-invasive alternative, and utilizes the patient’s own tissue to potentially heal the pars defect, as demonstrated by this case report.
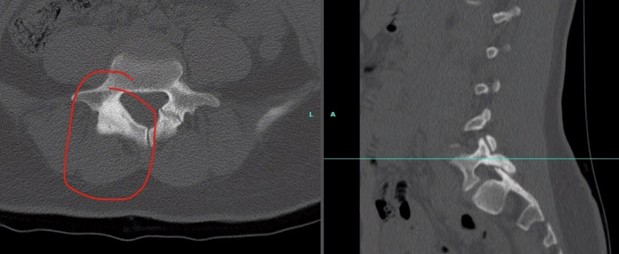
A 15-year-old female softball player presented with low back pain for almost two years and failed conservative management previously. The post BMAC injection she had demonstrated resolution of the pars defect via repeat CT scans three months post-procedure. Detecting spondylolysis early and using a less-invasive approach to treatment like BMAC injection, has the potential to regenerate the pars interarticularis and allow athletes to return to sport safely and successfully. Future studies are needed to further evaluate the power of BMAC in healing spondylolysis patients.
INTRODUCTION
Low back pain (LBP) is a frequent cause of sport limitation in young athletes and a common complaint that prompts a visit to a physician’s office. It is reported that up to half of adolescents experience low back pain, with rates being substantially higher in those who are active in sports (Calvo-Munoz et al. 2013) (Rossi and Dragoni 2001). The most common cause of low back pain in the adolescent athlete is isthmic spondylolysis, which is a defect of the pars interarticularis. The prevalence of isthmic spondylolysis is estimated to be 14-30% in adolescent athletes with LBP (Rossi and Dragoni 2001) (Mitchell et al. 2019). The pars acts as a bony strut, connecting the inferior and superior articulating processes of the vertebra to both the pedicle and lamina. The L5 vertebra serves at the point of maximal stress and is thus the most common location for this to occur (Kanter 2017). When both sides are involved, it can progress to spondylolisthesis, or anterior slippage of the vertebra, which can lead to serious neurological symptoms (Foreman 2012). Spondylolysis can be either congenital, where the patient is born without a bony connection, or traumatic, which in athletes is most often a repetitive microtrauma that leads to the defect over time (Foreman 2012).
Patients with spondylolysis will often present with pain that worsens with extension, increased pain with direct pressure to the spinous process at the level of the defect, limited range of motion of the lumbar spine or hypermobility, tightness of hamstrings and hip flexors, and referred pain to the buttocks or thigh but usually no radicular signs (Kanter 2017) (Lawrence et al. 2016).
The majority of patients with spondylolysis respond positively to bracing, stabilization and strengthening exercises, proper rest, and a gradual return to sport. Surgery is sometimes recommended in those individuals who are athletes, have had persistent low back pain for more than six months, who fail conservative management, or who experience no resolution of the pars fractures on imaging (Syrmou et al. 2010). Surgical techniques include a pedicle screw and hook, buck screw, u-rod technique, or scott wiring (Mohammed et al. 2017). Around 9-15% of symptomatic spondylolysis cases end up requiring surgery (Syrmou et al. 2010). Research is lacking on orthobiologics in assisting with pain and healing in spondylolysis, particularly in the young athlete. The aim of this case report is to present, share and discuss the case of using bone marrow aspirate concentrate to successfully treat a symptomatic pars defect with radiographic evidence of healing
CASE REPORT
A 15-year-old female with no significant past medical history who presented to the office for evaluation of lower back pain. She is a competitive year-round travel softball player and plays catcher. Her pain was described as ongoing for the last 1.5-2 years and did not improve after rest, bracing, and anti-inflammatory medications. The patient described the pain as achy, stabbing, and sharp at times. Furthermore, she had also been working with a physical therapist over the past few years to increase her hip strength. The PT noted she had weak glutes and strong hip flexors that they thought may be contributing to her back pain. The patient was also taking celecoxib since being diagnosed with a pars fracture in June 2020. She was evaluated by a spine surgeon who recommended she wear a TLSO brace until December 2020 and was told she would need a spinal fusion if she does not improve. The patient and her parents were trying to avoid surgical intervention due to her young age and active lifestyle. On initial presentation, her vitals were within normal limits. On physical examination, the patient's sensory to light touch was intact from L2-S1 bilaterally and Wharton's wheel revealed no sensory deficits. Reflexes were 2+ at L4 and S1 bilaterally. Lumbar inspection was negative for ecchymosis, swelling, bony deformity, or atrophy. Lumbar palpation was negative for warmth or soft tissue edema. The patient had tenderness to palpation at L4-L5 on the right side, but none on the left. It was noted that she had full range of motion in flexion and rotation, with pain reproduced on extension. Both the slump test and straight leg test were negative bilaterally. Differential diagnosis included lumbar strain, herniated disc, compression fracture, spinal stenosis, inflammatory spondyloarthropathy, spondylothesis, spondylolysis, malignancy, osteomyelitis.
TESTS/IMAGING
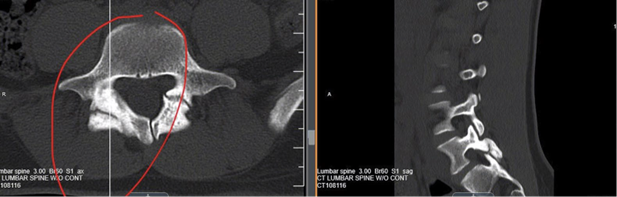
Initial assessment computerized tomography scan with axial cuts and sagittal reconstructions:
Procedure
On September 9, 2020, bone marrow aspiration at the iliac crests was performed using sterile technique and under ultrasound guidance . A total of 20cc of anesthetic were injected at the level of the periosteum. A Trocar/Vidacare OnControl System was then inserted at the level of the bone and advanced into the bone cavity. The stylet was then removed and ½-¾ cc’s containing a ratio of 1 mL of 5,000 U of Heparin to 4mL of normal saline was injected at each harvest site. A 10-12 cc syringe was then attached containing 5,000 U of Heparin and a total of 108cc of bone marrow was aspirated from bilateral iliac crests. The total nucleated cell count in syringe was 2.002 billion cells with 94% viability. The buffy coat was diluted at a ratio of 1:100 with a total volume of 7.1 cc and a TC20 count of 2.76 x 10^6. The lipid layer was diluted at a ratio of 1:50 with a total volume of 2.2 cc and a TC20 count of 6.42 x 10^5.
On the same day, later into the afternoon, the patient was injected with the bone marrow aspirate as described above under ultrasound and fluoroscopic guidance at the following sites:
Left L4-L5 facet 1.0 cc SD/PLM/SCP mixture
SD: Same day; PLM: Platelet lysate; SCP: Super concentrated platelets
Post-procedure imaging
After BMAC injection (12 weeks post-procedure):
DISCUSSION
In adults with degenerative disc disease (DDD), Elabd et al. demonstrated (2016) that intradiscal injection of autologous, hypoxic cultured bone marrow-derived MSCs in adult patients with chronic lower back pain is successful at improving quality of life, strength, and mobility. PRP has also been shown to be beneficial in the DDD population (Tuakli-Wosornu et al. 2016). However, there are virtually no regenerative medicine studies in the spondylolysis population, particularly in adolescent athletes. Spondylolysis has also been linked with Spina Bifida Occulta cases in patients, where a 2018 study found that out of 650 lumbar spine CT scans reviewed over a five-year period, 15% were found to have a pars defect present. The conclusions of the study revealed that “the occurrence of SBO within the group with a spondylolysis is much higher than in the group where no spondylolysis is present. There is a higher incidence of SBO in the younger patients with spondylolysis. 56% of pediatric patients with symptomatic spondylolysis will have SBO” (Vannet et al. 2018). The case report below explores a symptomatic spondylolysis patient who demonstrates the potential for bone marrow aspirate injections in healing the pars interarticularis defect and allowing athletes to return to sport successfully, quickly, and pain-free.
This case demonstrates a novel approach to treating spondylolysis in adolescent athletes who have failed conservative management. A typical treatment approach to treating spondylolysis is a facet joint injection with steroid and anesthetic, but this is only reported to be effective in less than 50% of patients (Kang et al. 2018). Surgery is another option, but surgery is invasive and can lead to serious complications and a prolonged recovery period, not ideal for competitive athletes. Bone marrow aspirate concentrate (BMAC) injection provides a safe, non-invasive alternative, and utilizes one’s own tissue to potentially heal the pars defect, as demonstrated by this case report. While studies have shown promising results when using stem cell therapies like BMAC for degenerative disc disease, hip and knee osteoarthritis, and chondral injuries (Chahla et al) (Whitney et al.2020), there are no formal studies on BMAC injections in treating spondylolysis. One case report by Mansfield et. al (date) [ref] of a 29-year-old male with bilateral spondylolysis showed significant pain reduction and increased range of motion at 5 weeks post BMAC injection. Another case report by Centeno et al. (date) [ref] revealed a 19-year-old wrestler who experienced improvement in pain, mobility, and resolution of the pars defect on CT scan after BMAC therapy, similar to our patient. To our knowledge, these are the only two cases of spondylolysis treated with advanced image-guided BMAC injection.
Bone marrow aspirate (BMA) serves as a source of several growth factors, including platelet-derived growth factor (PDGF), transforming growth factor–beta (TGF-β), and bone morphogenetic protein (BMP)–2 and BMP-7, which are known to have anti-inflammatory properties (Freitag et al. 2016) (Kolber et al.). It also contains mesenchymal and hematopoietic stem cells, which are responsible for cell immunomodulation, or a change in the body’s immune system. It is thought that stem cell therapy leads to suppression of the immune response, in turn reducing inflammation (Kolber et al.). Mesenchymal stem cells aid in skeletal tissue development, whereas hematopoietic stem cells play a critical role in the formation of blood cells. BMA is also involved in new vessel formation, which enhances tissue repair and regeneration in adults (Kolber et al.). These critical properties of BMA allow for the potential of healing bone, as we observed in this case with resolution of the pars defect on repeat CT scan three months post-injection.
Our patient in this study was a competitive softball player, a sport that is often overlooked for this type of injury. Mitchell et al. reviewed the medical charts of 1,025 adolescent athletes with LBP and discovered that softball had the third-highest prevalence of spondylolysis for females. The repetitive extension and rotation movements involved in throwing cause compressive and shear forces through the lumbar spine, particularly in the position of catcher, which in theory may increase the risk of spondylolysis injury. Over time, if the pars defect is left untreated, this leads to weakness of surrounding structures and puts patients at risk of progression to spondylothesis, which can be much more serious and lead to serious neurological compromise. While surgery is an option in patients who fail conservative management, it is not without cost. In Overley et al.’s meta-analysis, it was discovered that out of 74 operative patients, 15 experienced perioperative complications. Detecting spondylolysis early and using a less-invasive approach to treatment like BMAC injection, has the potential to regenerate the pars interarticularis and allow athletes to return to sport safely and successfully. Future studies are needed to further evaluate the power of BMAC in healing spondylolysis patients.
Written informed consent was obtained from the patient for publication of this Case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
REFERENCES
- Calvo-Muñoz I, Gómez-Conesa A, Sánchez-Meca J. Prevalence of low back pain in children and adolescents: a meta-analysis. BMC Pediatr. 2013;13:14. Published 2013 Jan 26. doi:10.1186/1471-2431-13-14
- Rossi, F. & Dragoni, S.. (2001). The prevalence of spondylolysis and spondylolisthesis in symptomatic elite athletes: Radiographic findings. Radiography. 7. 37-42. 10.1053/radi.2000.0299.
- Selhorst, Mitchell DPT, OCS*; Fischer, Anastasia MD†; MacDonald, James MD, MPH† Prevalence of Spondylolysis in Symptomatic Adolescent Athletes: An Assessment of Sport Risk in Nonelite Athletes, Clinical Journal of Sport Medicine: September 2019 - Volume 29 - Issue 5 - p 421-425 doi: 10.1097/JSM.0000000000000546.
- Kanter A.S., McDowell M.M. (2017) Repair of Pars Defects and Spondylosis. In: Holly L., Anderson P. (eds) Essentials of Spinal Stabilization. Springer, Cham. https://doi.org/10.1007/978-3-319-59713-3_23.
- Foreman P, Griessenauer CJ, Watanabe K, Conklin M, Shoja MM, Rozzelle CJ, et al. L5 spondylolysis/spondylolisthesis: a comprehensive review with an anatomic focus. Childs Nerv Syst. 2013;29(2):209–16.
- Lawrence KJ, Elser T, Stromberg R. Lumbar spondylolysis in the adolescent athlete. Physical Therapy in Sport. https://www.sciencedirect.com/science/article/pii/S1466853X16300037. Published April 13, 2016.
- Tuakli-Wosornu YA, Terry A, Boachie-Adjei K, et al. Lumbar Intradiskal Platelet-Rich Plasma (PRP) Injections: A Prospective, Double-Blind, Randomized Controlled Study. PM&R. https://www.sciencedirect.com/science/article/pii/S1934148215009715. Published August 24, 2015.
- Campbell RSD, Grainger AJ, Hide IG, et al. Juvenile spondylolysis: a comparative analysis of CT, SPECT and MRI. Skeletal Radiol 2005; 34:63–73.
- Syrmou E, Tsitsopoulos PP, Marinopoulos D, Tsonidis C, Anagnostopoulos I, Tsitsopoulos PD. Spondylolysis: a review and reappraisal. Hippokratia. 2010;14(1):17-21.
- Mohammed N, Patra DP, Narayan V, Savardekar AR, Dossani RH, Bollam P, Bir S, Nanda A. A comparison of the techniques of direct pars interarticularis repairs for spondylolysis and low-grade spondylolisthesis: a meta-analysis. Neurosurg Focus. 2018 Jan;44(1):E10. doi: 10.3171/2017.11.FOCUS17581. PMID: 29290131.
- Elabd C, Centeno CJ, Schultz JR, Lutz G, Ichim T, Silva FJ. Intra-discal injection of autologous, hypoxic cultured bone marrow-derived mesenchymal stem cells in five patients with chronic lower back pain: a long-term safety and feasibility study. Journal of Translational Medicine. https://link.springer.com/article/10.1186/s12967-016-1015-5. Published September 1, 2016.
- Vannet N, Ahuja S, Davies P, et al. INCIDENCE OF PARS DEFECT ASSOCIATED WITH SPINA BIFIDA. Orthopaedic Proceedings. https://online.boneandjoint.org.uk/doi/abs/10.1302/0301-620X.92BSUPP_IV.0920569a. Published February 21, 2018.
- Kang WY, Lee JW, Lee E, Kang Y, Ahn JM, Kang HS. Efficacy and outcome predictors of fluoroscopy-guided facet joint injection for spondylolysis. Skeletal Radiology. https://link.springer.com/article/10.1007/s00256-018-2897-5. Published February 2, 2018.
- Chahla J, Dean CS, Moatshe G, Pascual-Garrido C, Serra Cruz R, LaPrade RF. Concentrated Bone Marrow Aspirate for the Treatment of Chondral Injuries and Osteoarthritis of the Knee: A Systematic Review of Outcomes. Orthopaedic journal of sports medicine. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4714134/. Published January 13, 2016.
- Whitney KE, Briggs KK, Chamness C, et al. Bone Marrow Concentrate Injection Treatment Improves Short-term Outcomes in Symptomatic Hip Osteoarthritis Patients: A Pilot Study. Orthopaedic journal of sports medicine. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7731709/. Published December 9, 2020.
- Mansfied JT, Miller B, Desai M. Fluoroscopic-guided Medicinal Signaling Cells Injection for the Treatment of Bilateral Spondylolysis: A Case Report [abstract]. PM R. 2019; 11(S2)(suppl 2). https://pmrjabstracts.org/abstract/fluoroscopic-guided-medicinal-signaling-cells-injection-for-the-treatment-of-bilateral-spondylolysis-a-case-report/. Accessed May 31, 2021.
- Chris Centeno MD. spondylolysis treatment options. Regenexx. https://regenexx.com/blog/spondylolysis-treatment-options/#gref. Published January 24, 2020. Accessed May 31, 2021.
- Freitag J, Bates D, Boyd R, et al. Mesenchymal stem cell therapy in the treatment of osteoarthritis: reparative pathways, safety and efficacy – a review. BMC Musculoskeletal Disorders. https://link.springer.com/article/10.1186/s12891-016-1085-9. Published May 26, 2016.
- Kolber, Morey J. PT, PhD, CSCS*D1; Purita, Joseph MD2; Sterling, Bryan BS1; Stermer, Jaclyn BS1; Salamh, Paul DPT, PhD3; Masaracchio, Michael PT, PhD, OCS, SCS4; Hanney, William J. DPT, PhD, ATC, CSCS5 Stem Cell Injections for Musculoskeletal Pathology: An Overview for the Sports Medicine Professional, Strength and Conditioning Journal: December 2019 - Volume 41 - Issue 6 - p 75-86 doi: 10.1519/SSC.0000000000000500.
- Overley SC, McAnany SJ, Kim J, et al. Return to Play in Adolescent Athletes With Symptomatic Spondylolysis Without Listhesis: A Meta-Analysis - Samuel C. Overley, Steven J. McAnany, Steve Andelman, Jun Kim, Robert K. Merrill, Samuel K. Cho, Sheeraz A. Qureshi, Andrew C. Hecht, 2018. SAGE Journals. https://journals.sagepub.com/doi/full/10.1177/2192568217734520. Published October 5, 2017.






